The reference and training app for the Vortex Approach has been released (free of any charge!) on the iTunes App Store. Link to check it out by clicking the image:
Warm thanks and congratulation to Nicholas Crimes for this excellent work.
SASA is again leading the way with their highly interactive app for mobile devices at the current national conference, and have now added OpenAirway to the fold! Conference attendees, speakers and trade representatives have immediate access to this #FOAM resource, directly in the conference app. Well done and thanks for the support!
Reproduced here with credit to GomerBlog, because “To laugh at oneself is the beginning of wisdom”.
Without getting into a lengthy argument about what constitutes a second-generation supraglottic airway (or an extraglottic vs. supraglottic, for that matter), if you are using an SGA with a gastric drainage port (such as the LMA Proseal, LMA Supreme, i-Gel, etc) you have a very simple and easy conduit to insert a mid-oesophageal thermistor probe to monitor patient temperature.

Ideally, to achieve a mid-oesophageal position, you need the probe to extend 5-10 cm past the tip of the SGA, so try and remember to measure the probe against the device before insertion and mark it with a small piece of dressing tape. This has an added advantage of helping prevent air leak via the drainage tube if your SGA is not seated or strapped ideally. Of course, this means that drainage via the oespophageal lumen is significantly impaired, and you cannot insert a gastric tube without removing the probe first, so it is only suited to patients in whom you have little concern regarding reflux and aspiration. Devices that offer twin drainage tubes (such as the 3gLM) are a way around this problem.
Rigid endoscopes are very valuable tools for intubation in certain difficult scenarios, but are not commonly used in most centres. The techniques and learning curve differ significantly from normal direct laryngoscopy, requiring independent practice to become proficient. Pictured here are (left to right) a rigid bronchoscope, Bonfils, Levitan and Shikani optical stylets (rigid intubating endoscopes).
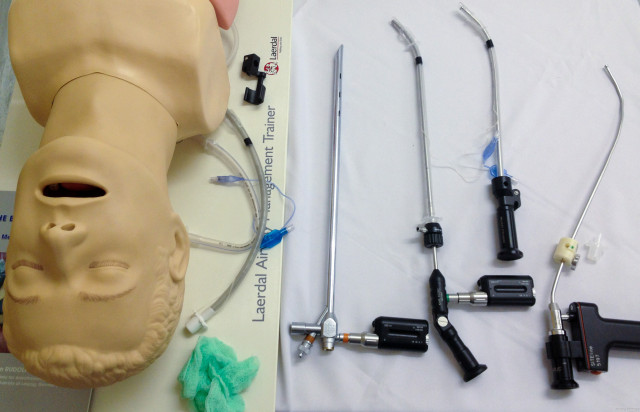
This is the set-up for basic training on an UCT Anaesthesia Airways course. Which of these devices have you used? Do you have tricks or comments to share?
Great post on EMDocs covering useful airway techniques, which is helpfully referenced. Not really fair calling the concepts ‘novel’, as most have been around for some time, but are certainly not in ubiquitous use!
Click here for the post…and kudos to Joe Rodgers and EMDocs for the good work 🙂
Good suggestion out of the Twittersphere from @Sub_Effect – the Difficult Airway Society (DAS) has a smartphone app available for both iOS and Android which allows you to work through the various algorithms at the click of a thumb. iDAS includes the following algorithms:

Best bit? It’s free!
Kudos to Yen Chow (@TBayEDGuy) for alerting us to these two useful instructional clips on the HQMedEd page:
Time to get down and bougie?
Intubation in a young child with a severe submandibular abscess using the paediatric Bonfils rigid intubating endoscope under inhalational general anaesthesia. Direct laryngoscopy showed only severe swelling with a Cormack-Lehane grade 3b view. A standard laryngoscope was used with the left hand to create an open path for the Bonfils just right of the midline, avoiding the worst of the submandibular swelling. 3.5mm Bonfils allowed intubation with a 4.5 mm uncuffed ETT. Note that because this is a rigid intubating scope, it is not inserted through the vocal cords, but they are visible through the tube as it is inserted with the Bonfils held steady.
http://youtu.be/fPpdhg_DxnY
Nice illustration of the various lung volumes and capacities courtesy of www.medicomic.com. Easy aide memoire: a capacity is always the sum of two or more volumes. Note that the absolute volumes reflected here would be for a normal sized adult.