“Dual endoscopy” refers to using two devices – usually a video laryngoscope and a rigid or flexible endoscope – to manage an airway. The Bonfils (or Shikani or Levitan) optical stylet is often used in this context. Performing dual endoscopy provides “three levels of protection”:
- If the glottic opening is easily seen with the laryngoscope, the rigid endoscope simply acts as an ideally shaped or steerable stylet to introduce the tube
- If the view is poor (CL grade 3 or 4), the laryngoscope can be used to guide the tip of the ETT and endoscope “into the ballpark”, and then the final positioning of the tip of the tube through the vocal cords is achieved with the endoscope.
- If the airway is badly soiled or swollen (eg. ongoing bleeding or angioedema), the endoscope can be used as a lightwand for a transillumination technique. (Remember lightwands, anyone?)
Here’s a brief informal video explaining the first two points, using the CMAC VL/VS:
Another dual endoscopy approach is “VAFI” (video-assisted flexible/fibreoptic intubation), where a VL is used to help place a flexible endoscope, whereafter the rest of the intubation is continued using the flexible. Several good case reports of this technique are described in the literature.
Here’s a brief clinical example of dual endoscopy using the CMAC VL and VS (video stylet). This case was performed for teaching purposes, rather than a difficult airway. Note the endoscopic view appearing as a picture-in-picture is from the editing; the images are on two separate displays. (It starts a little late due to the author forgetting to press the record button on the device).
Some of the newest devices (eg. CMAC 8404; Glidescope Core monitors) allow both images to be displayed on the screen simultaneously, either as a “picture in picture” view, or side by side. If using the latter, orientating the images so that the VL is on the left and endoscope on the right is convenient, as this matches the two hands being used. Here’s an example, again in a patient with an easy airway, but simulating CL3 view:
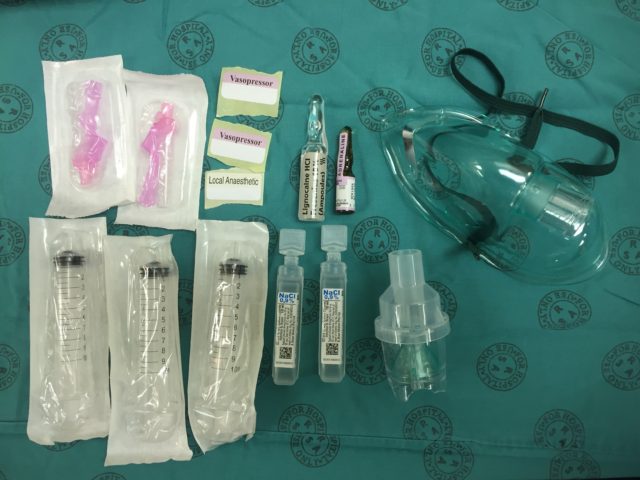
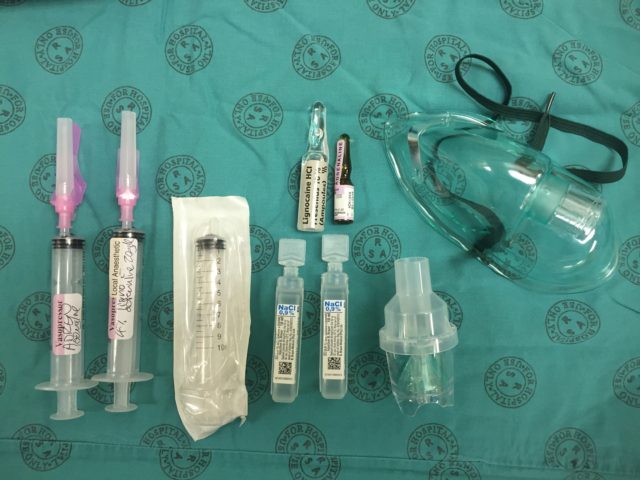
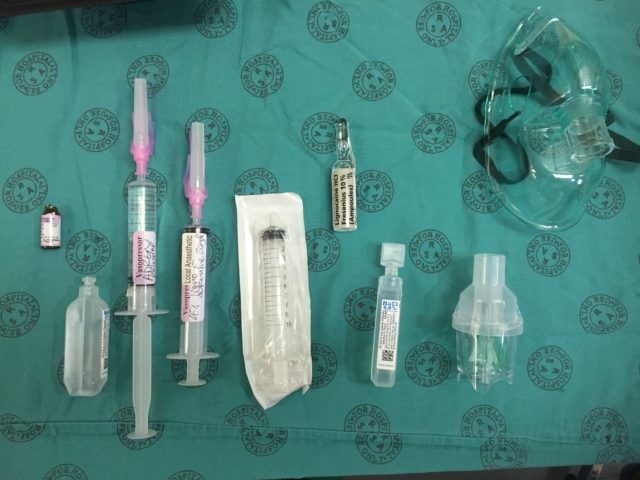 Transfer 2 ml (200 mcg) of the dilute adrenaline into the mix syringe:
Transfer 2 ml (200 mcg) of the dilute adrenaline into the mix syringe:  Add 4 ml of the 10 % lignocaine solution to the mix syringe (use all 5 ml if you want to make a 5 % solution rather than the usual 4 %):
Add 4 ml of the 10 % lignocaine solution to the mix syringe (use all 5 ml if you want to make a 5 % solution rather than the usual 4 %):  Add saline to the mix syringe to a total volume of 10 ml. You now have 4 % (or 5 %) lignocaine with 20 mcg/ml adrenaline:
Add saline to the mix syringe to a total volume of 10 ml. You now have 4 % (or 5 %) lignocaine with 20 mcg/ml adrenaline: 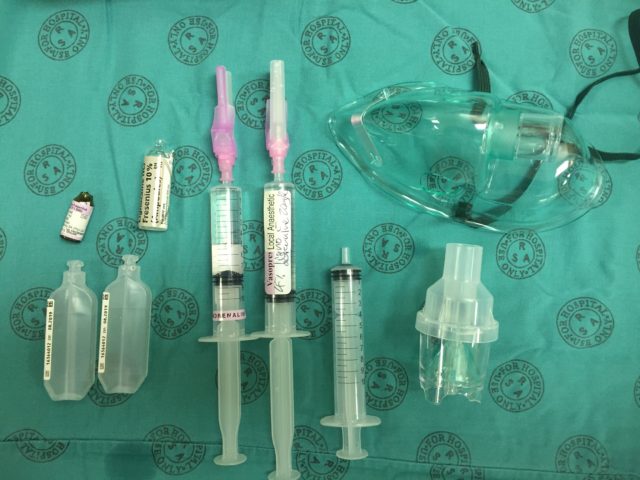
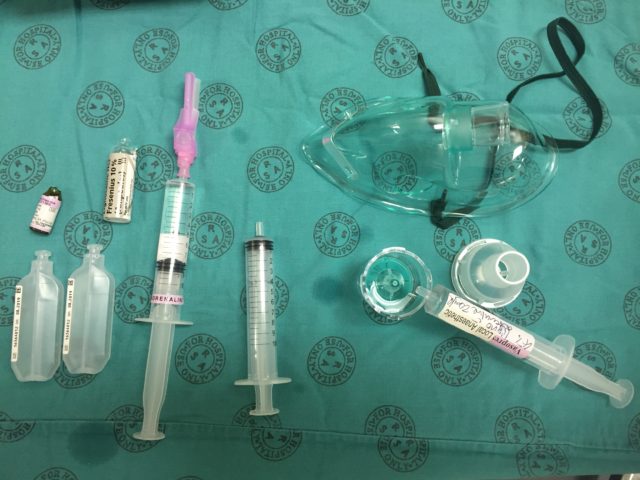 Split the remaining 5 ml mixture into two 10 ml syringes (using your third syringe) to be used for spray-as-you-go through the scope if needed:
Split the remaining 5 ml mixture into two 10 ml syringes (using your third syringe) to be used for spray-as-you-go through the scope if needed: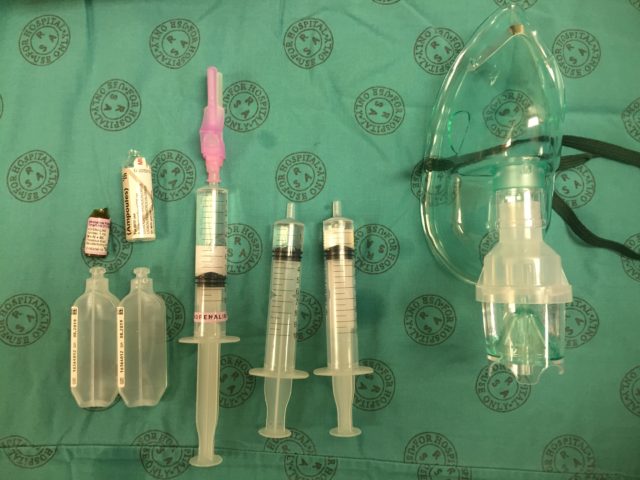 Put the rest of the adrenaline solution somewhere safe (or discard it), and draw back the plungers on the mix syringes all the way. This introduces air which then blows the local mix through the scope when you do spray-as-you-go. Don’t forget to give the neb plenty of time to work (15-20 minutes, until complete).
Put the rest of the adrenaline solution somewhere safe (or discard it), and draw back the plungers on the mix syringes all the way. This introduces air which then blows the local mix through the scope when you do spray-as-you-go. Don’t forget to give the neb plenty of time to work (15-20 minutes, until complete).  Don’t forget to use adjuvant strategies to improve your topicalisation, such as gargling, atomised spray, or topical gel/paste, and enter your cases into a registry such as TheAirwayApp so that we can build worldwide experience with different techniques!
Don’t forget to use adjuvant strategies to improve your topicalisation, such as gargling, atomised spray, or topical gel/paste, and enter your cases into a registry such as TheAirwayApp so that we can build worldwide experience with different techniques!