As promised/per usual, here’s my presentation from the current National Assembly on Paediatric Emergency Medicine, being held now (16-19 Feb 2017) at the Apollo Institute of Medical Sciences & Research, Hyderabad, India. Much of the content is in the audio, of course…which I will post if/when available.
Comments welcome below as usual!
Category Archives: Algorithms
Algorithms page updated
It’s always a challenge to stay up to date in the field of airway management, but we do try. The recently published All Indian Difficult Airway Association Guidelines (just released in the December 2016 edition of IJA) have been added to our Algorithms page, as well as an update of the Vortex 2 video and revised links to the Resuscitation Council of South Africa algorithms. If you spot missing algorithms or broken links, please comment!
Cape Town FCA2 Refresher: DAS 2015 Guidelines
Here’s the excellent simulation/re-enactment video from Simpact on the Elaine Bromiley Case that I featured in the lecture.
You can download my accompanying lecture notes on the DAS 2015 guidelines here:
FCA2 Refresher 2016 Notes – Hofmeyr – Difficult Airway Society 2015 Guidelines
Frerk et al’s article on the 2015 guidelines is available from the BJA here (open access), and the excellent recent editorial on front-of-neck access by Timmerman, Chrimes and Hagberg is here. This is not in the notes, as it has only just been published online.
The links to the different algorithms are on the Algorithms page, or you can browse the DAS website.
The surgical airway technique video that woudn’t play is below.
OAA/DAS Guidelines for Difficult & Failed Intubation in Obstetrics!
Hot of the press – the Obstetric Anaesthetists’ Association and Difficult Airway Society have released their combined guidelines on difficult and failed intubation in obstetrics, which are freely available from Anaesthesia online.
- Click here for the online publication
- Click here to access the PDF
- Click here to read the accompanying editorial by Rucklidge and Yentis
The guidelines are presented as a ‘Master Algorithm’ and several sub-algorithms to deal with specific aspects of obstetric airway management, and a guide to making the decision to awake the patient or continue with surgical delivery after an airway event:
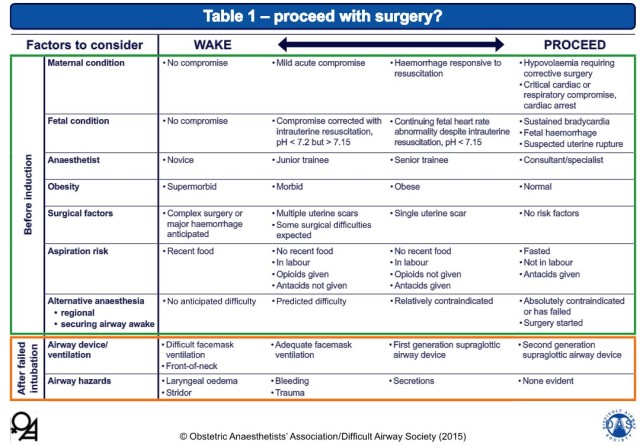
Some thoughts (COI – the author did provide feedback on the draft algorithms):
- Stressing good positioning for airway management is absolutely critical in this population, and especially in practice environments where patients tend to have a high BMI (a common situation in our South African setting). The guidelines include ramping and the ear-to-sternal-notch (E2SN) position.
- The inclusion of cricoid pressure will inevitably spark the usual debate, but it is this author’s contention that this is likely an appropriate use until more evidence to the contrary emerges. The guidance to consider CP reduction or release in the event of difficulty is apt.
- The inclusion of gentle face-mask assisted ventilation during RSI is a welcome inclusion. Will we see NPO2 or HFNC included in later editions as more outcomes evidence emerges?
- Advocating the use of VL in obstetrics certainly sounds like a good idea, but is not attainable for most of the developing world. This is a huge area for growth/research – the development of low-cost VL solutions.
This is a great step forward in promoting safe airway management and guiding training in a particularly dangerous corner of our practice.
For some more thoughts and images, here is a Prezi on the subject presented at the SASA Difficult Airway workshop in 2014:
Difficult Face Mask Ventilation – ATOTW 321
The newest edition of the Anaesthesia Tutorial of the Week (ATOTW #321) covers the much underestimated but critically important topic of predicting and managing difficulty in face mask ventilation. Irish anaesthetists Jonathan Holland and Will Donaldson have created a useful resource for anyone studying or performing airway management, or refreshing for exam purposes.
ATOTW is a free resource created and hosted by the World Federation of Societies of Anaesthesiologists. You can sign up to receive the weekly mails here, and download this edition on mask ventilation here:
ATOTW 321 – Difficult Mask Ventilation
The authors discuss the predictors of difficult mask ventilation and report/propose another two mnemonics, to add to the existing stable (MOANS, BONES, etc):
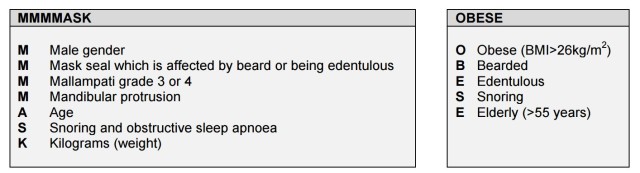
I’ve always used MOANS for mask factors (like I use LEMON for laryngoscopy), but all these mnemonics cover the same ground. MOANS, for instance, stands for
- M Mask seal factors, like beards, NGTs, odd shaped faces
- O Obesity and causes of Obstruction, like tumours/angioedema
- A Age extremes (the elderly and very young)
- N No teeth (or nasty dentition)
- S Snoring and Stiff lungs (the latter being issues like inhalation burns and acute bronchospasm, where the higher pressures required increase the risk of gastric insufflation and Splinting of the diaphragm)
As you can see, they are all much the same, although there are a few things that are not covered by every algorithm. The purist would point out that obesity is defined as a BMI of >30 kg/m2, not 26 as stated in the table.

The authors then present a useful flowchart for addressing unexpected difficulty, which is quite sensible. It is much in line with the DAS guidelines and other algorithms for general airway difficulty, and useful for instruction. Of course, in a dire emergency, using a cognitive aid such as the Vortex would be effective.
New ANZCA Difficult Airway Cognitive Aid
Thanks to the inimitable Dr Nicholas Crimes for this great resource. Very pleasing to see a good collection of algorithms in the appendices of the document, in the spirit that we have tried to create here. 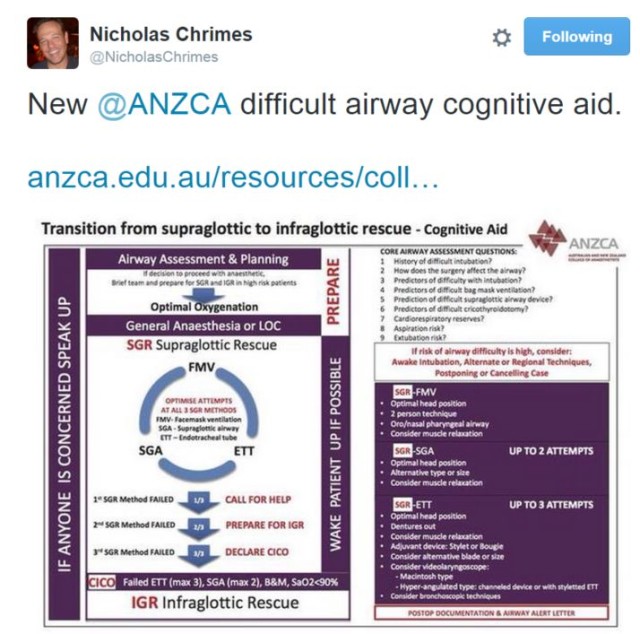
A more thorough review to follow, but it is usually hard to fault our Antipodean friends.
Emergency Paediatric Intubation for the Infrequent Intubator
Presentation for the 19th World Congress of Disaster and Emergency Medicine (combined with EMSSA 2015) in Cape Town. Click on the fullscreen icon to see it in a more appropriate aspect ratio
Vortex Approach App Released!
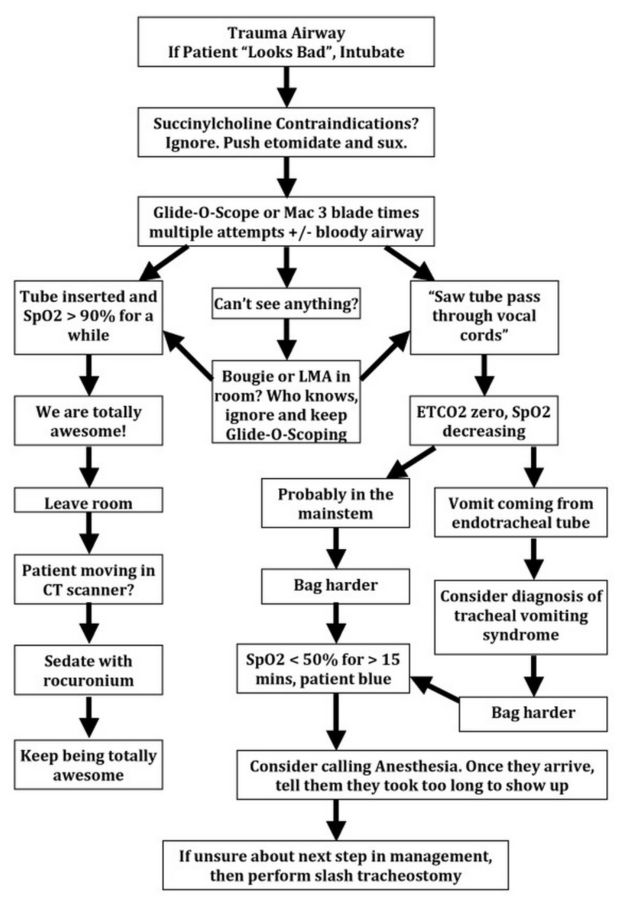
New Gomerblog Trauma Airway Algorithm
Reproduced here with credit to GomerBlog, because “To laugh at oneself is the beginning of wisdom”.
Difficult Airway Society Algorithm App
Good suggestion out of the Twittersphere from @Sub_Effect – the Difficult Airway Society (DAS) has a smartphone app available for both iOS and Android which allows you to work through the various algorithms at the click of a thumb. iDAS includes the following algorithms:
- RSI Failed Intubation
- CICV
- Routine Failed Intubation
- Overview of Guidelines

Best bit? It’s free!