A quick video aimed at introducing our clinicians to a new piece of equipment, but potentially a useful overview of this type of device to anyone who may make use of portable flexible ‘scopes.
A quick video aimed at introducing our clinicians to a new piece of equipment, but potentially a useful overview of this type of device to anyone who may make use of portable flexible ‘scopes.
…to come and have great fun on our courses at UCT. This from the hands-on airway endoscopy afternoon run recently for the Department of Anaesthesia’s own staff:
Two and a half minutes to quickly bring you up to speed on the anatomy of a flexible intubating endoscope:

This month’s edition of Anesthesiology News features a worthwhile piece from Prof John Doyle, in which he poses 7 questions on the current state of airway management to 6 airway experts from around the world (Abdelmalak, Cooper, Frova, Rosenblatt, Spiegel and Doyle himself), and collates their responses into a dialogue. Definitely worth reading to determine what some (certainly not all) of the biggest names in the world are thinking on:
You can read the article on the Anesthesiology News site by clicking here or the image above, or download the PDF version here.
For what it is worth, here are my own answers, distilled into one-liners. I’m very willing to enter into discussions about them!
There are a lot of excellent (and complementary) views expressed in the article, which are worth reading. Check it out!
Rigid endoscopes are very valuable tools for intubation in certain difficult scenarios, but are not commonly used in most centres. The techniques and learning curve differ significantly from normal direct laryngoscopy, requiring independent practice to become proficient. Pictured here are (left to right) a rigid bronchoscope, Bonfils, Levitan and Shikani optical stylets (rigid intubating endoscopes).
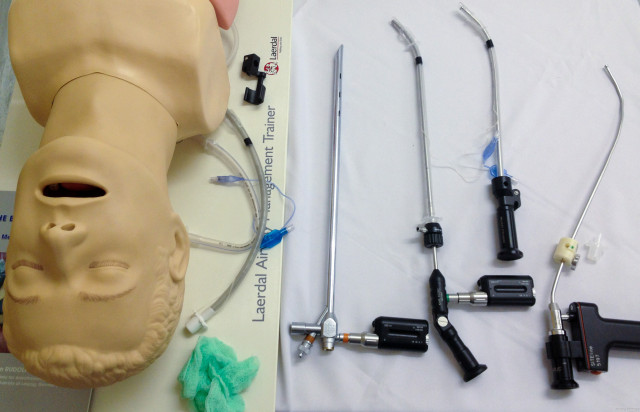
This is the set-up for basic training on an UCT Anaesthesia Airways course. Which of these devices have you used? Do you have tricks or comments to share?
Intubation in a young child with a severe submandibular abscess using the paediatric Bonfils rigid intubating endoscope under inhalational general anaesthesia. Direct laryngoscopy showed only severe swelling with a Cormack-Lehane grade 3b view. A standard laryngoscope was used with the left hand to create an open path for the Bonfils just right of the midline, avoiding the worst of the submandibular swelling. 3.5mm Bonfils allowed intubation with a 4.5 mm uncuffed ETT. Note that because this is a rigid intubating scope, it is not inserted through the vocal cords, but they are visible through the tube as it is inserted with the Bonfils held steady.
http://youtu.be/fPpdhg_DxnY
https://www.youtube.com/watch?v=Mbg1VHRD350
Flexible fibreoptic and video endoscopes are fantastic but expensive pieces of equipment. In order to be maintained in top working condition, they need a little tender loving care. A particular problem occurs when the sheath of the scope becomes damaged or cracked, allowing fluid (especially corrosive cleaning solutions) to enter the inner workings of the scope, causing irreparable damage. The inner workings of the scope are a sealed environment. The patency of the seal – and thus the presence or absence of any damage – can easily be determined by performing a leak test. Although this is usually performed by medical technologists who are looking after the scopes, it can just as be performed quickly by the user while the scope is being prepared, or just before cleaning. Spend 100 seconds watching this brief, unadorned video which will walk you through the process. The demonstration here is using our Storz equipment, but is very similar regardless of the make or model of endoscope.
https://www.youtube.com/watch?v=n5XyA4NagMQ
@fibroanestesia comes up with some interesting ideas. Here they use a combination of the AScope3 (a disposable flexible video endoscope) and the King Vision video laryngoscope to perform a highly controlled intubation in a patient with an intrathoracic goitre. They have obviously pre-assessed this patient and concluded that the risk of failed intubation or positional loss of the intrathoracic airway due to compression is minimal.
Blinded intubation through the 3gLM SGA, as viewed by a video endoscope riding inside a Parker Flex-Tip ETT.